Enhancing experience and access at the touch of a button
While recovering at home from your hip arthroscopy, you hear a ping coming from your cell phone – it’s a response to your questions about the pain medication you were prescribed. The response didn’t come from your physician or another member of your clinical team, it came from Felix – an artificial intelligence (AI) chatbot.
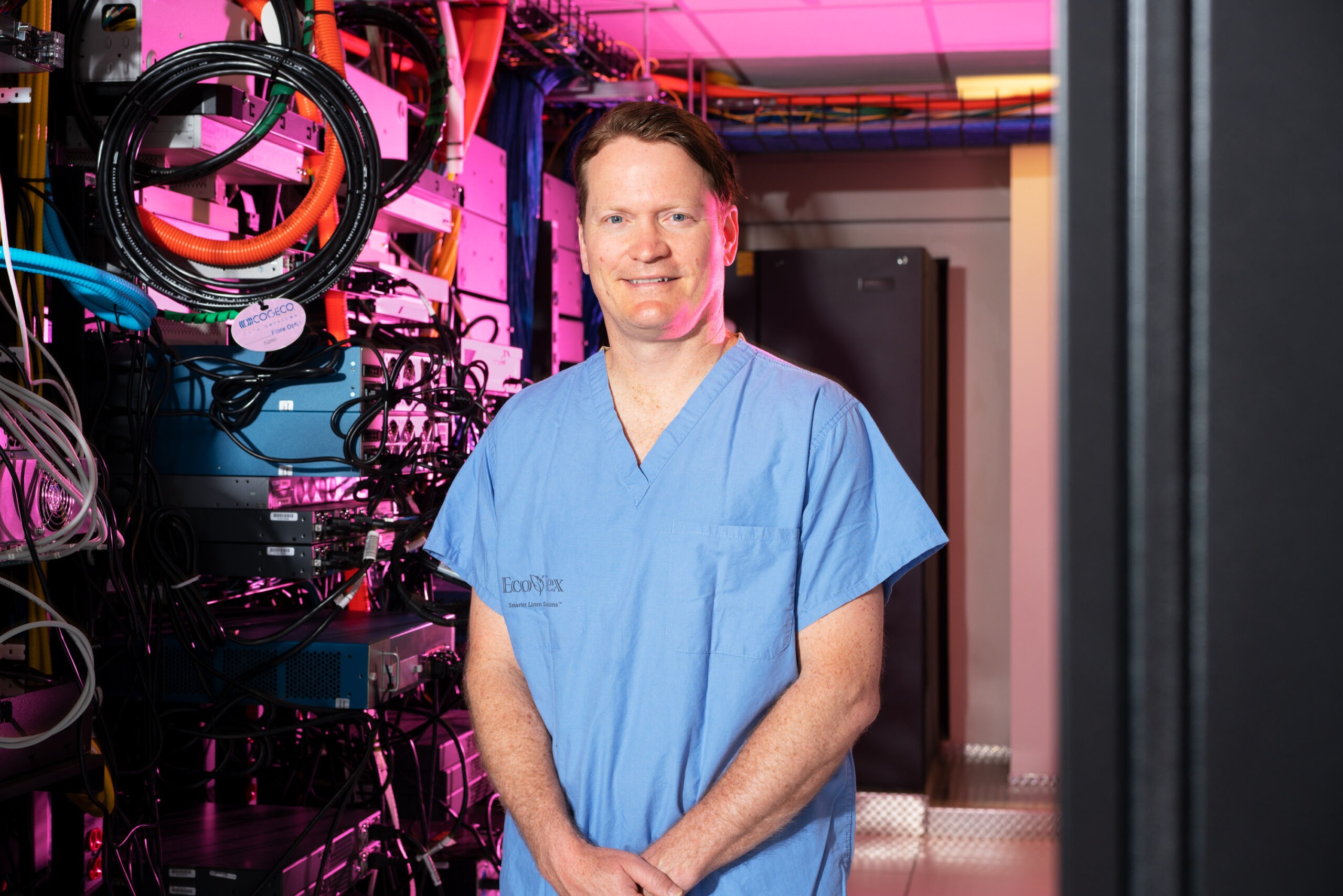
This was the experience of patients enrolled in Canada’s first study on post-operative recovery supported by a chatbot. “The Department of Surgery at Women’s College Hospital (WCH) was an early adopter of virtual care, using tools like automated text reminders and photo sharing, and while helpful it has added pressure to healthcare resources. So, we wanted to look for additional ways to support patients as they recover, while respecting concerns like workload and time,” says Dr. Tim Dwyer, a WCH surgeon and the study lead.
Working with a technology company, the research team developed content allowing Felix to send patients automated reminders for pain management and wound management, as well as instructions for physiotherapy and rehabilitation specific to hip arthroscopy. As an AI chatbot, Felix was also designed to independently respond to common post-surgical questions posed by patients. The study found that Felix handled roughly 79 per cent of all questions appropriately by either addressing and interacting with the patient directly or by facilitating contact with the care team.
“While hip arthroscopy is a relatively common and routine surgery, we know that patients are often nervous when they go home to recover,” Dr. Dwyer explains. “As a result, they typically have numerous questions about their recovery, making sure they are healing correctly or following the required physiotherapy. Felix helped alleviate many of their concerns.”
Participants enrolled in the study overwhelmingly liked the additional support provided by the chatbot, highlighting that it improved their care experience. They also expressed no concern about the safety of using a chatbot to support their recovery.
“We were surprised by the results, to be honest,” Dr. Dwyer says. “Patients felt more supported and appreciated the immediacy of the response from Felix. AI is advancing quickly and further refining its accuracy. Going forward, I think we will see a greater use of chatbots during post-surgical recovery. Not as a replacement to post-operative in-person visits, but as an added element to enhance the patient experience.”
Digital health tools and virtual care models have also allowed WCH to make strides forward in access to care, particularly within mental health. “Roughly five per cent of all adults in Canada reported being diagnosed with PTSD or post-traumatic stress disorder by a healthcare provider,” says Dr. Dana Ross a WCH psychiatrist and researcher specializing in trauma therapy. “Of those who sought professional help, four in five had trouble accessing the healthcare services they needed. Unfortunately, there are simply not enough trained therapists to meet the need.”
In response, Dr. Ross and her team knew that they needed to move beyond the traditional in-person therapy model and began two research initiatives focused on advancing safe and timely access to care. “Our first project is the Trauma Portal. We developed an online platform where participants complete eight self-paced learning modules and participate in weekly group video sessions. The content for the platform was leveraged from our Resourced and Resilient - or R&R- program for stage one trauma therapy at the hospital.”
What started as a pilot study has now grown into a randomized control trial with multiple patient cohorts. “We needed to understand the useability, efficacy, and accessibility of online trauma therapy first. Our initial results were very promising. Not only did participants find that their PTSD symptoms improved but they had no safety concerns and typically stayed with the program from start to finish,” Dr. Ross explains. The research team also found that participants enjoyed being able to take the modules at their own pace, pausing when needed, and at a time that best suited them. The trial is expected to be completed at the end of this year with WCH beginning to offer the Trauma Portal clinically in 2024. “Going forward, patients that are referred to our trauma therapy program can access the Trauma Portal within weeks – allowing them to receive mental healthcare when they need it, not many months later.”
The second research project led by Dr. Ross is Community R&R, whereby multidisciplinary healthcare workers from local hospitals, community health centres and family health teams, licensed in psychotherapy, receive virtual self-paced training from WCH, so that they can begin to offer stage one trauma therapy to their patients and clients. When the partner sites in the study begin to offer the R&R group to patients, the facilitators receive support in the form of weekly virtual supervision from experienced trauma therapists at WCH. Like the Trauma Portal project, Community R&R continues to grow – beginning with five community partner sites and expanding to fifteen additional sites later this year.
“Both research projects have significant potential to be spread and scaled across the province,” Dr. Ross noted. “In future phases of our studies, we believe that other mental health programs across the province can implement these initiatives to grow both the pool of therapists available and provide alternative or new models of care to address wait times.”
Another initiative leveraging new approaches to care is the At-Home Transcranial Direct Current Stimulation for Depression in Pregnancy Study led by Dr. Simone Vigod, head of the Department of Psychiatry and a senior scientist at WCH. “Depression during pregnancy is common. But for many of our patients talk therapy isn’t enough,” explains Dr. Vigod. “Their symptoms are more severe, however, they are often not comfortable taking antidepressant medication. We know that leaving depression untreated can have significant consequences for both the parent and the development of the fetus.”
Looking for new forms of treatment, Dr. Vigod and her collaborators at Sunnybrook Research Institute and the Centre for Addiction and Mental Health launched a randomized controlled trial to determine if transcranial direct current stimulation (tDCS), a form of noninvasive brain stimulation, works to relieve depression in pregnant individuals not on medication. Through a headband placed onto the scalp, tDCS stimulates parts of the brain directly associated with depression with the aim of resetting or reregulating the brain. While tDCS has never been used to address depression during pregnancy before, it has been used clinically for many years for depression, as well as other conditions.

“The tDCS device is small and easy to use. It takes 30 minutes each day for three weeks and is done while the participant is awake and sitting down at home,” says Dr. Vigod. “The stimulation is very localized, so no other regions of the brain are affected. People often ask me what it feels like, you can hardly feel it at all. In our original study, most people simply felt a bit of buzzing sensation.”
To ensure that participants feel supported and comfortable using the tDCS device at home, they are first asked to come into the hospital to learn how to use it. Then, for each day at home, the participant is connected virtually to the research team who monitors their use of the device. They receive a specific code electronically to unlock the device and begin treatment. The code is only good for that day, which means it cannot be used more frequently or for longer than is prescribed.
While still in the first year of recruitment, the response from patients has been positive so far. “They like it a lot, find it easy to use and have been able to integrate it into their everyday routine,” says Dr. Vigod. “If proven to be effective, tDCS has the potential to dramatically expand the treatment options available to patients struggling with depression during pregnancy. If we are committed to enhancing access to healthcare, then we need to be willing to do things differently, test new ideas and implement novel evidence-based care models.” By using virtual care as a tool, not an end in itself, clinicians and scientists at Women’s College Hospital are addressing issues like access, wait times and patient experience.
“Access does not always mean quality,” says Dr. Ibukun Abejirinde, a WCH scientist specializing in virtual care and health equity. As an AMS Research Fellow in Compassion and Artificial Intelligence, Abejirinde is researching how newcomers, specifically refugees and landed immigrants, experience virtual primary care and the extent to which they view virtual care as compassionate. “Since COVID-19, many patients have their initial healthcare visit virtually. Although this has enabled access to care, when we look at underserved patient populations like newcomers, our initial research has shown that their expectations with respect to its quality is nuanced,” Abejirinde explains.
Over the past few years, most care providers have found a balance between virtual appointments versus when in-person care is required. However, in this new era of digital health tools, there are still many questions that remain. This includes what equitable access to virtual care looks like – are there people who have limited access to virtual tools or who are falling through the cracks? How can providers ensure they are using tools that truly meet the needs of their patients?